Post-Discharge Care Coordination for Skilled Nursing Facilities
The Landing System for
Skilled Nursing Discharges.
The EHR manages the flight. MAXMRJ manages the landing.
Your coordinators' 30-60 minute referral process — done. Free to start. No credit card. No IT project.

Post-Discharge Follow-Up
Don't Fly Blind.
Once they discharge, they fall off your radar.
Nearly 1 in 5 patients are readmitted (Crash).
Readmission Risks lead to CMS Penalties and reduced VBP reimbursements—protect your facility with post-discharge care coordination software.
Clear the Fog.
Land Safely.
How MAXMRJ Prevents SNF Readmissions
MAXMRJ acts as the Landing System for post-acute care. We merge discharging patients and community resources into a single visibility layer.
Care Traffic Control
Discharge Logistics Coordination
Coordinate Nursing, DME, and Transport from one command tower. Eliminate phone tag forever.
Risk Radar
Proactive AI Risk Analysis
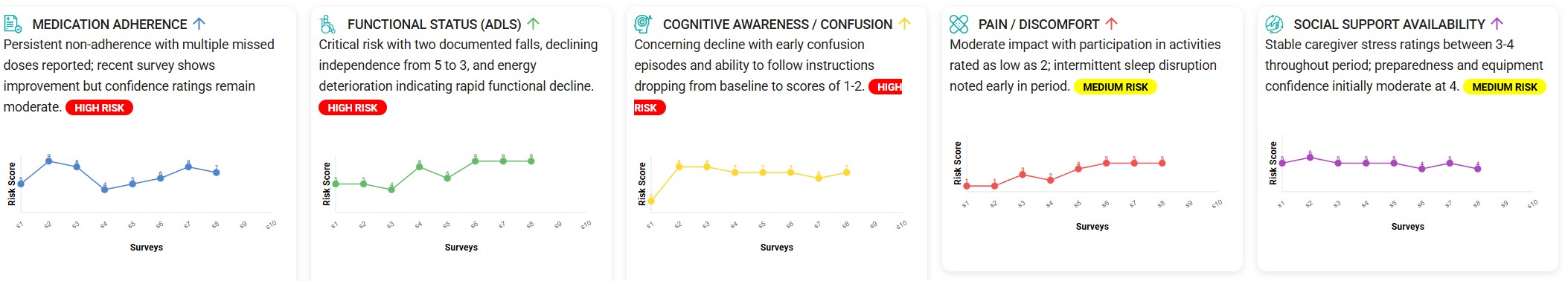
After discharge, automated surveys go to patients or caregivers. AI analyzes responses over time to flag potential concerns before they become emergencies.
Provider Network
Community Provider Coordination
Connect directly to community providers ready to serve your discharged patients.
From Discharge to Done in 4 Steps
Replace 30-60 minutes of phone tag with a streamlined digital workflow.
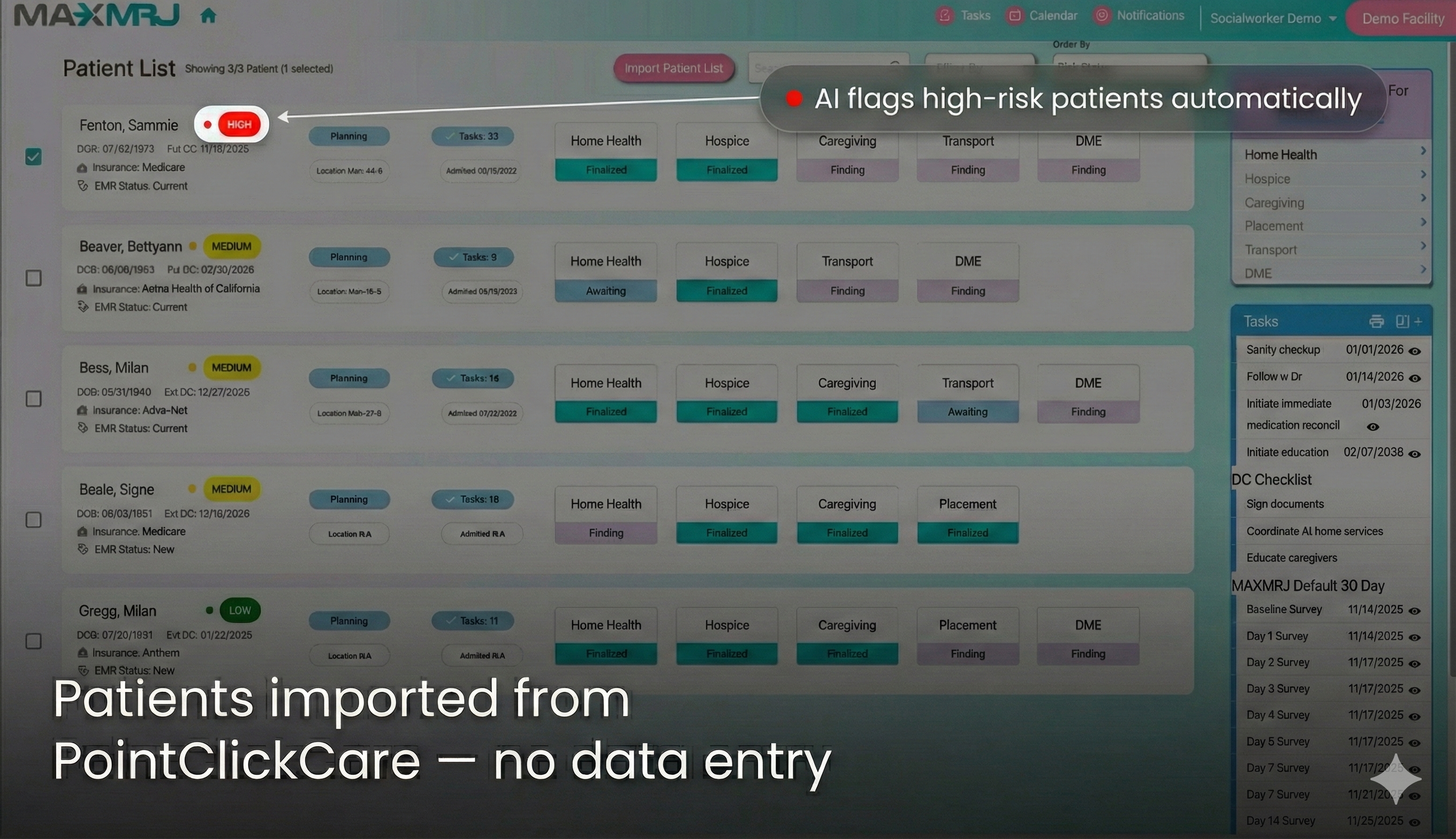
Patient Selected from PointClickCare
Patient details and discharge information flow automatically. No re-entering data.
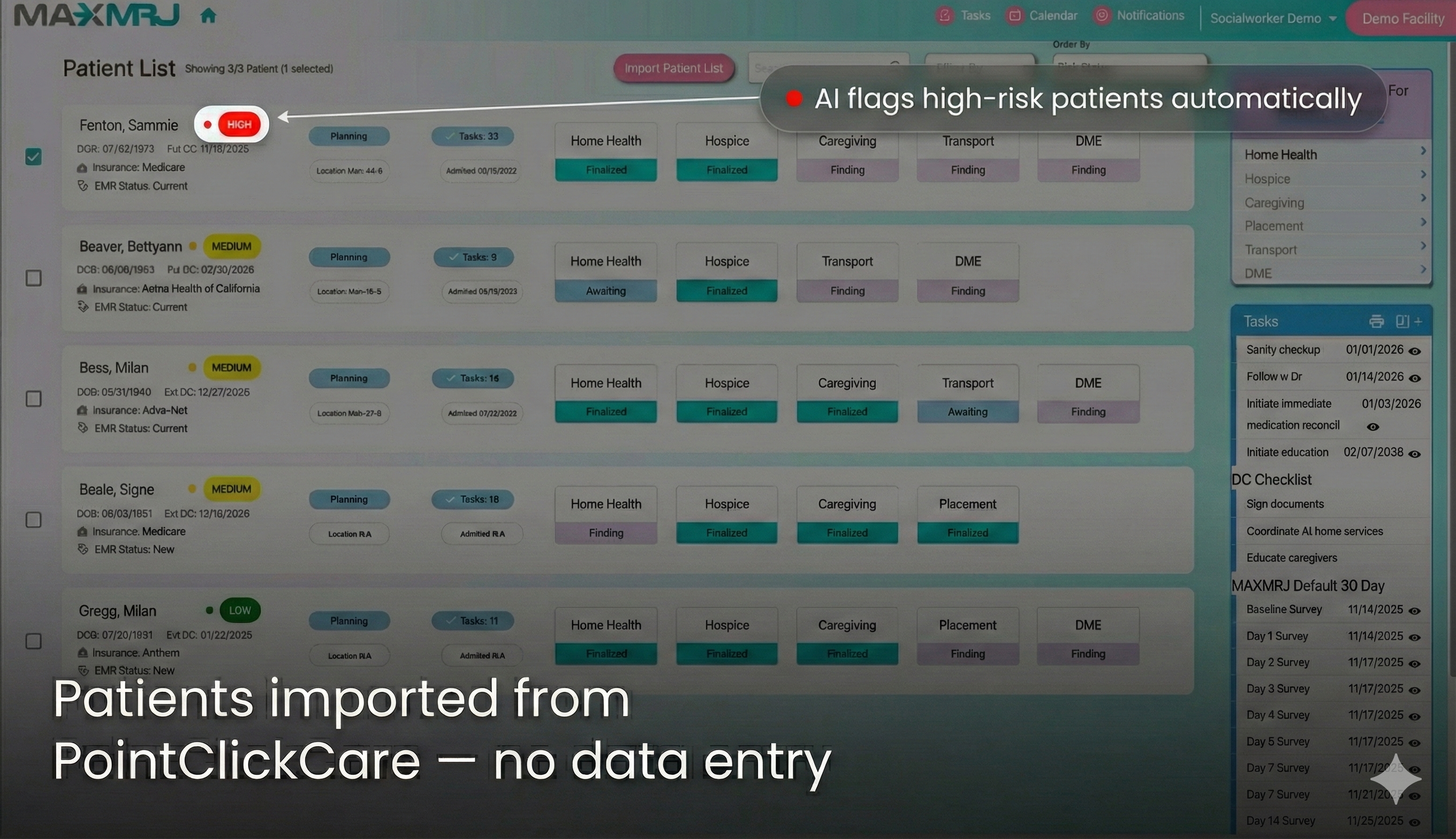
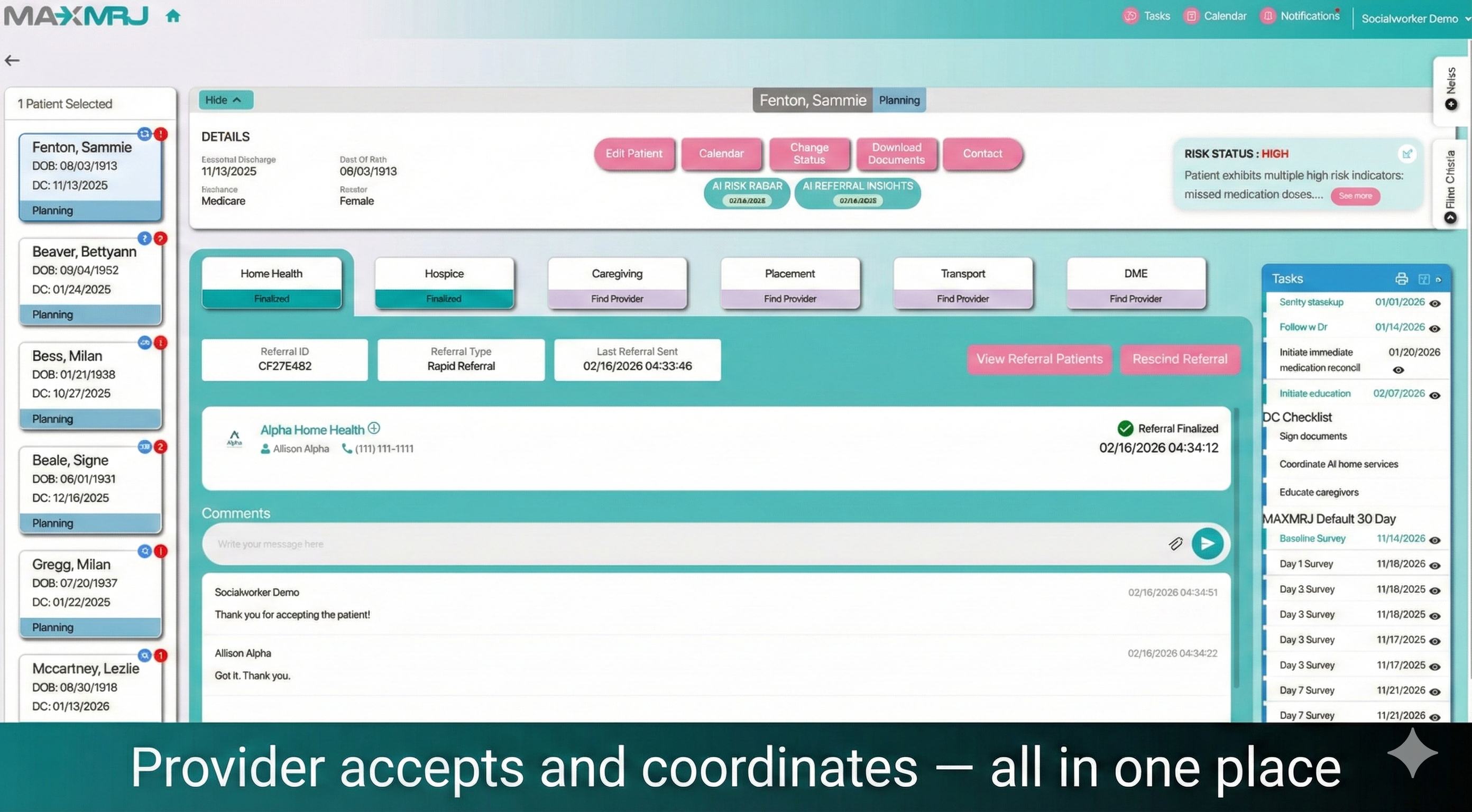
Choose Providers — One Click
Select from your network: home health, DME, transport, hospice. All notified simultaneously.
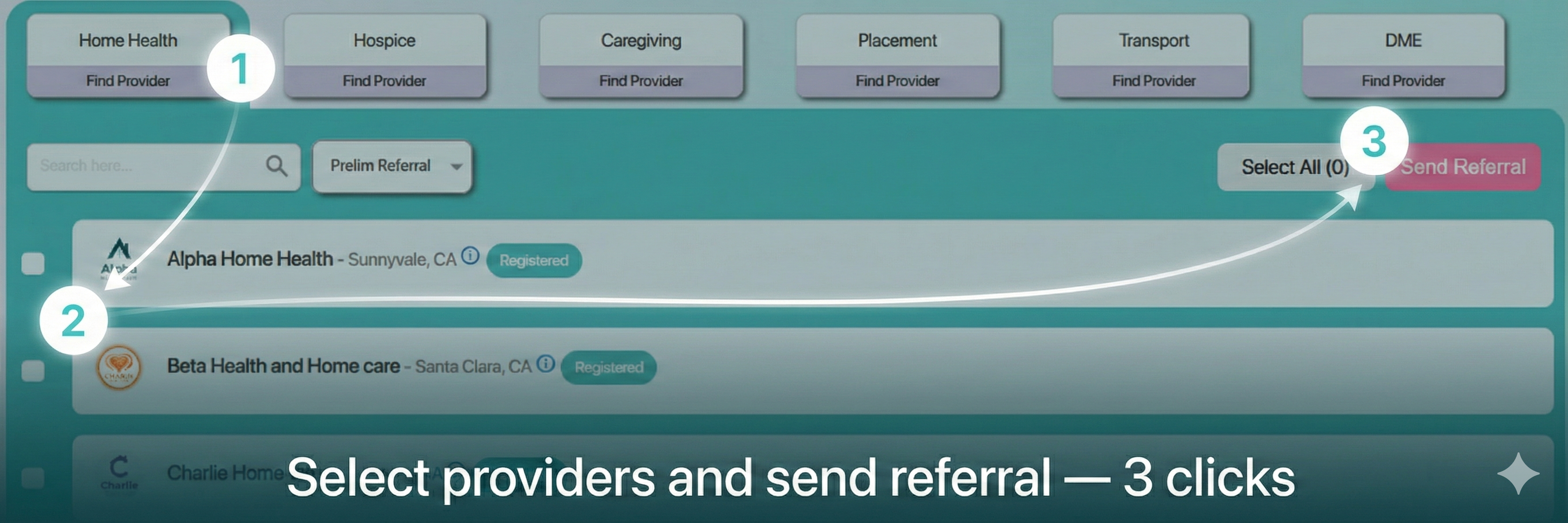
Providers Respond and Coordinate
Providers accept, share documents, coordinate in MAXMRJ. Full visibility for your coordinator.
Follow Up After DischargeAI Add-on
Automated surveys go to the patient or caregiver at home. AI analyzes responses over time to flag potential concerns — and gives your coordinator specific recommendations.
What VBP Penalties Are Costing You
CMS withholds 2% of your Medicare revenue and redistributes based on quality. 71.7% of SNFs (nearly 3 in 4) received penalties in 2024.
In FY2025, 100% of your VBP score is based on your 30-day readmission rate.
Source: CMS SNF VBP Program public data. Individual results vary by facility.
The Math That Matters
A 120-bed SNF generating ~$3.45M in Medicare revenue has a $69K VBP pool (2% withhold).
The average penalized SNF loses ~$17,000/year from that pool.*
MAXMRJ AI follow-up: $349/month = $4,188/year.
Moving from penalized to neutral territory: $17K–$34K annual VBP benefit. Add coordinator efficiency savings (free platform) and the math compounds.
The base coordination platform is free. You're only paying for the AI follow-up that catches problems before they become readmissions.
* Sources: CMS FY2025 SNF VBP Final Rule; Wheeler et al., JAGS 2025 (71.7% penalized); MedPAC 2024. Average penalty ~$10K–$22K. Individual results vary. MAXMRJ does not guarantee specific outcomes.
Why MAXMRJ (Not Another Feature Inside Your EHR)
Your EHR (e.g. PointClickCare)
- Manages the patient while they're in your facility
- Tracks data inside your walls
- No post-discharge coordination or follow-up
MAXMRJ (After They Leave)
- Coordinates the 2-5 external providers your patient needs at home
- Checks in with patients and caregivers after discharge
- AI flags concerns early so your team can act
These are different problems. They need different tools. That's why we integrate WITH PCC, not compete against it.
“We already have social workers calling patients after discharge.”
Great — MAXMRJ doesn't replace that relationship. It makes it systematic.
Instead of calling 30 discharged patients and hoping to catch problems, your coordinator sees exactly which 5 patients need attention today.
The human touch stays. The guesswork goes.
Hospitals Are Now Choosing SNFs Based on Outcomes
Under CMS's TEAM Bundled Payment Model, hospitals own the financial risk for 30 days after discharge — covering Medicare Part A and B costs including your SNF stay, home health, and readmissions. Especially for SNFs admitting orthopedic, surgical, or cardiac patients, they'll partner with facilities that can prove good outcomes.
What Changed
Under TEAM, CMS bundles payment from surgery through 30 days post-hospital discharge — covering the majority of Medicare Part A and B costs, including SNF stays, home health, outpatient therapy, and readmissions. If a patient goes to your SNF and then gets readmitted to the hospital, the hospital pays the price.
That means hospitals are now actively evaluating which SNFs to partner with. Facilities that can demonstrate smooth transitions and strong post-discharge follow-up become preferred referral partners. Facilities that can't? They lose referrals.
Year 1 is upside-only — no hospital owes money in 2026. But hospitals are already modeling 2027, when two-sided financial risk kicks in. The SNFs building relationships now will be the preferred partners when the stakes are real.
80%
of Medicare SNF-to-home patients had no structured post-discharge support — hospitals have no outcome data on most of their discharge partners
30 days
Hospitals bear Medicare costs for 30 days post-discharge — including your SNF stay, home health, and any readmissions back to the hospital
2027
Downside risk begins. Hospitals are vetting preferred SNF partners now — before the financial stakes are real
A Day in the Life of Your Coordinator
See how MAXMRJ transforms the discharge workflow.
Protect Your VBP Scores.
Help prevent readmissions by standardizing your discharge logistics.
Upgrade Your Intake.
Get listed in SNF networks and receive referrals directly. AI-powered intake summaries help you process referrals faster.
What Our Partners Say
“MAXMRJ cut our referral process from over an hour to just a few minutes.”
Director of Social Services
200-bed SNF